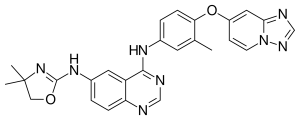
Tucatinib (Tucaxen), a tyrosine kinase inhibitor, specifically targets and inhibits the activity of HER2, a protein overexpressed in HER2-positive breast cancer cells, effectively halting their growth and proliferation. It’s precisely targeted and inhibits HER2 activity, effectively hindering the growth and proliferation of cancer cells.
Tucatinib’s approval and utilization primarily occur in the context of metastatic breast cancer, where the disease has spread beyond the initial site to other parts of the body. To bolster its effectiveness in tackling the advanced stages of HER2-positive breast cancer, Tucatinib (Tucaxen) is often synergistically employed alongside other therapeutic agents, encompassing targeted therapies and chemotherapy.
The rationale behind using tucatinib lies in its ability to interfere with the signaling pathways associated with HER2, which play a crucial role in the growth and survival of cancer cells. By inhibiting these pathways, tucatinib aims to suppress the progression of the disease and improve patient outcomes.
It is important to note that the landscape of medical research and drug development is dynamic, and new information may have emerged since my last update. To stay abreast of the latest information on Tucatinib (Tucaxen), including its evolving applications, potential side effects, and ongoing clinical trials, it is crucial to consult with healthcare professionals or refer to reputable medical resources and the most recent scientific literature.
Introduction of Tucatinib (Tucaxen):
In the relentless pursuit of innovative solutions for cancer treatment, the pharmaceutical landscape has witnessed remarkable strides, with Tucatinib (Tucaxen) emerging as a beacon of hope in the realm of targeted therapies. Tucatinib, a small molecule inhibitor, has garnered significant attention for its potential to revolutionize the treatment landscape for certain types of cancer, particularly those associated with overexpression of human epidermal growth factor receptor 2 (HER2). This article explores the intricacies of Tucatinib, shedding light on its mechanism of action, clinical applications, and the transformative impact it promises in the ongoing battle against cancer.
HER2-positive cancers, characterized by the overexpression of the HER2 protein, represent a subset of malignancies associated with aggressive progression and poorer prognosis. Tucatinib, also known by its trade name Tukysa, stands out as a novel tyrosine kinase inhibitor designed to selectively target and inhibit the activity of HER2, thereby disrupting the signaling pathways that drive cancer growth and survival.
The unique feature distinguishing Tucatinib from its predecessors lies in its ability to cross the blood-brain barrier, a formidable obstacle in the treatment of metastatic brain lesions associated with HER2-positive breast cancer. This characteristic renders Tucatinib particularly promising for patients who have experienced metastasis to the central nervous system, providing a much-needed therapeutic option in a traditionally challenging treatment landscape.
As we delve into the depths of Tucatinib’s molecular intricacies, clinical trial outcomes, and real-world applications, a comprehensive understanding of this groundbreaking therapy will unfold. Join us on a journey through the scientific and clinical landscape of Tucatinib, where precision meets promise in the pursuit of more effective and targeted cancer treatments.
Background of Tucatinib (Tucaxen):
Tucatinib (Tucaxen), a potent and selective tyrosine kinase inhibitor, has emerged as a beacon of hope in the evolving landscape of cancer therapeutics. The development of this groundbreaking compound stems from a critical need to address the challenges posed by HER2-positive cancers, a subset notorious for its aggressive nature and limited treatment options.
Human epidermal growth factor receptor 2 (HER2), a transmembrane protein, plays a pivotal role in regulating cell growth and differentiation. However, when HER2 becomes overexpressed or amplified, it can contribute to uncontrolled cell proliferation and increased aggressiveness of certain cancer types, including breast, colorectal, and gastric cancers. HER2-positive breast cancer, in particular, has been associated with a more aggressive disease course and poorer prognosis.
Recognizing the urgent need for targeted therapies to combat HER2-positive cancers, researchers embarked on the journey to develop Tucatinib (Tucaxen).
This meticulously crafted small molecule inhibitor specifically targets the HER2 receptor’s tyrosine kinase domain, effectively disrupting the signaling pathways that drive uncontrolled cancer proliferation. Unlike some earlier HER2-targeted therapies, Tucatinib exhibits a remarkable specificity, minimizing off-target effects and enhancing its therapeutic efficacy.
One of the notable challenges in treating HER2-positive breast cancer is the occurrence of metastasis to the brain, which significantly complicates treatment strategies. Traditional HER2 inhibitors have struggled to penetrate the blood-brain barrier effectively, limiting their impact on metastatic lesions in the central nervous system. Tucatinib, however, has demonstrated a unique ability to traverse this barrier, making it a game-changer in the management of HER2-positive breast cancer with brain metastases.
The journey of Tucatinib (Tucaxen) from conception to clinical reality has been marked by rigorous research, preclinical studies, and extensive clinical trials. Its development reflects a collaborative effort between pharmaceutical innovators, clinicians, and researchers committed to advancing the field of oncology. As we delve deeper into the nuances of Tucatinib’s development, mechanism of action, and clinical applications, a clearer picture will emerge of the significant strides this compound has made in addressing the unmet needs of patients with HER2-positive cancers.
Mechanism of Action Tucatinib (Tucaxen):
Tucatinib (Tucaxen), distinguished by its precision in targeting the human epidermal growth factor receptor 2 (HER2), operates as a formidable force against the relentless progression of HER2-positive cancers. Within the intricate cellular realm, Tucatinib orchestrates a molecular ballet, meticulously disrupting the aberrant signaling pathways that fuel uncontrolled cell growth and proliferation.
At the heart of Tucatinib’s efficacy is its role as a tyrosine kinase inhibitor, a class of compounds designed to interfere with the activity of enzymes crucial in cell signaling. HER2, a member of the HER family of receptors, is a tyrosine kinase receptor known for its involvement in promoting cell division and growth. In HER2-positive cancers, the overexpression or amplification of HER2 leads to hyperactivated signaling pathways, fostering the aggressive behavior of cancer cells.
Tucatinib’s specificity lies in its ability to selectively target the tyrosine kinase domain of the HER2 receptor. By binding to this critical region.
Tucatinib (Tucaxen) inhibits the enzymatic activity of HER2, disrupting the downstream signaling cascades that fuel cancer progression. This targeted approach minimizes collateral damage to healthy cells and tissues. A key advantage in mitigating side effects commonly associated with non-specific treatments.
Moreover, Tucatinib’s unique capability to penetrate the blood-brain barrier sets it apart from its predecessors. This feature is of paramount significance in the context of HER2-positive breast cancer. Where metastasis to the brain poses a formidable challenge. Tucatinib’s ability to reach metastatic lesions in the central nervous system enhances its efficacy in addressing the intricate landscape of HER2-positive cancers with brain involvement.
The multifaceted nature of Tucatinib’s mechanism of action not only halts the unbridled proliferation of cancer cells but also holds promise in circumventing resistance mechanisms that may arise during the course of treatment. As ongoing research continues to unravel the complexities of Tucatinib’s impact at the molecular level, its role as a targeted therapy stands as a testament to the evolving precision medicine paradigm in the fight against HER2-positive cancers.
Clinical Uses of Tucatinib (Tucaxen):
Tucatinib (Tucaxen) heralded as a breakthrough in targeted cancer therapy, has demonstrated remarkable clinical utility. Particularly in the management of HER2-positive breast cancer. The precision of its mechanism of action has paved the way for a spectrum of clinical applications. Offering renewed hope to patients facing the challenges posed by HER2 overexpression.
HER2-Positive Breast Cancer:
Tucatinib’s primary clinical use is in the treatment of HER2-positive breast cancer. This includes both early-stage and metastatic breast cancer cases where the overexpression of HER2 is a driving factor in disease progression. Notably. Tucatinib (Tucaxen) has exhibited efficacy in patients who have experienced metastasis to the brain, a historically challenging aspect of HER2-positive breast cancer treatment.
Metastatic Brain Lesions:
One of the distinguishing features of Tucatinib (Tucaxen) is its ability to penetrate the blood-brain barrier effectively. This unique characteristic has positioned Tucatinib as a valuable therapeutic option for patients with HER2-positive breast cancer metastasized to the brain. The drug’s capacity to reach and act on central nervous system lesions addresses a critical unmet need in the field of oncology. Providing new avenues for managing brain metastases.
Combination Therapies:
Tucatinib (Tucaxen) has demonstrated synergistic effects in combination with other HER2-targeted therapies and standard chemotherapy regimens. Combination approaches aim to maximize the therapeutic impact on HER2-positive cancers while potentially minimizing the development of resistance. Ongoing clinical trials explore the optimal combinations and sequences of treatments to enhance overall patient outcomes.
Clinical Trials in Other HER2-Positive Cancers:
Beyond breast cancer, ongoing clinical trials are investigating the efficacy of Tucatinib in other HER2-positive malignancies. Such as colorectal and gastric cancers. The outcomes of these trials hold the promise of expanding Tucatinib’s clinical footprint. Offering new treatment options for patients with diverse HER2-driven tumors.
Resistance Reversal Potential:
Tucatinib’s role extends beyond the initial treatment phases. With ongoing research exploring its potential to overcome resistance mechanisms that may develop during the course of therapy. This resistance reversal property positions Tucatinib as a valuable asset in the armamentarium against HER2-positive cancers. Providing a dynamic and adaptable approach to treatment.
As Tucatinib (Tucaxen) continues to undergo rigorous evaluation in clinical settings. Its expanding repertoire of clinical uses underscores its potential to redefine the treatment landscape for HER2-positive cancers. The ongoing exploration of combination therapies. Extension into other cancer types holds the promise of further elevating Tucatinib’s role in the evolving paradigm of precision oncology.