Baricitinib (Baricinix 2), a Janus kinase (JAK) inhibitor, has emerged as a transformative force in the treatment landscape of rheumatoid arthritis (RA). Approved by regulatory agencies around the world, including the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA). Baricitinib has redefined the approach to managing this chronic autoimmune disorder.
This article explores the nuanced details of Baricitinib’smechanism of action and clinical efficacy. Its evolving role in the ever-expanding toolkit for rheumatoid arthritis therapy.
Introduction of Baricitinib (Baricinix):
Rheumatoid arthritis (RA), is a chronic autoimmune disorder characterized by joint inflammation and systemic complications. Has long presented a formidable challenge to both patients and clinicians. In the dynamic landscape of rheumatology, the emergence of Baricitinib marks a significant milestone. Offering a novel and targeted approach to the treatment of this debilitating condition. Approved by regulatory agencies globally, Baricitinib has rapidly become a cornerstone in the therapeutic arsenal against RA. This article delves into the intricate details of Baricitinib (Baricinix 2). Exploring its mechanism of action, clinical efficacy, safety profile, and its expanding role in the broader landscape of autoimmune diseases.
Unravelling the Molecular Tapestry: Baricitinib’s Mechanism of Action:
At the forefront of Baricitinib’s prowess is its unique mechanism of action. As a Janus kinase (JAK) inhibitor, Baricitinib selectively targets JAK1 and JAK2. Integral components of the inflammatory signalling pathways implicated in rheumatoid arthritis. By intervening in these pathways. Baricitinib (Baricinix 2) effectively modulates the immune response. Offering a precision-engineered solution to the dysregulated inflammation at the core of RA pathology.
Clinical Efficacy in Rheumatoid Arthritis:
Clinical trials have borne witness to Baricitinib’s profound efficacy in the management of RA. Whether employed as a monotherapy or in conjunction with conventional disease-modifying antirheumatic drugs (DMARDs) such as methotrexate. Baricitinib demonstrates a rapid onset of action and significant improvements in disease activity. Joint function and overall quality of life. Its impact extends to inhibiting radiographic progression. Heralding a new era with the goal of altering the course of the disease.
Navigating the Safety Landscape:
While the therapeutic benefits of Baricitinib are apparent, an understanding of its safety profile is paramount. Adverse events, including upper respiratory tract infections and headaches, are observed, necessitating a careful balance between efficacy and potential risks. Vigilant monitoring and awareness of potentially serious events, such as infections and thrombosis, guide the judicious use of this innovative therapeutic agent.
Beyond Rheumatoid Arthritis: Expanding Horizons:
The story of Baricitinib transcends the confines of rheumatoid arthritis. Ongoing research endeavours to explore its potential applications in systemic lupus erythematosus, atopic dermatitis, and other autoimmune conditions. The versatility of Baricitinib underscores its potential to reshape the landscape of inflammatory disease management beyond the boundaries of RA.
A Glimpse into the Future: Ongoing Research and Evolution:
As the journey of Baricitinib unfolds, the landscape of rheumatoid arthritis therapy is undergoing a transformative shift. Ongoing research endeavours, comparative effectiveness studies, and real-world evidence contribute to the evolving narrative of Baricitinib’s role in clinical practice. The promise of continued innovation and refinement solidifies Baricitinib’s standing as a pivotal player in the dynamic and evolving field of autoimmune disease treatment.
In navigating the complexities of rheumatoid arthritis, Baricitinib emerges as a beacon of hope, offering not just relief from symptoms but a paradigm shift in the approach to disease modification. Its unique mechanism, clinical efficacy, safety considerations, and expanding horizons collectively paint a portrait of a revolutionary breakthrough that is reshaping the landscape of autoimmune disease therapeutics.
Background of Baricitinib (Baricinix):
The genesis of Baricitinib finds its roots in the persistent quest for more effective and targeted therapies for rheumatoid arthritis (RA), a chronic autoimmune disorder that intricately weaves joint inflammation and systemic complications into the lives of those affected. The background of Baricitinib is marked by a convergence of scientific understanding, technological advancements, and the unmet needs of patients grappling with the complexities of RA.
Rheumatoid Arthritis: A Complex Mosaic of Inflammation:
Rheumatoid arthritis, is characterized by immune system dysfunction leading to chronic inflammation in the joints. Has historically posed challenges in achieving sustained disease control. Traditional treatments include disease-modifying antirheumatic drugs (DMARDs) and anti-inflammatory medications. While offering relief, often falls short in altering the trajectory of the disease. The relentless pursuit of more effective therapies for RA laid the groundwork for the exploration of innovative approaches. Leading to the emergence of Baricitinib (Baricinix 2).
The Janus Kinase (JAK) Signaling Pathway: A Pivotal Discovery:
At the heart of Baricitinib’s development lies a pivotal discovery in the realm of molecular biology—the Janus kinase (JAK) signalling pathway. This intricate network of intracellular communication plays a crucial role in the regulation of immune responses. Recognizing the centrality of JAK1 and JAK2 in the inflammatory processes implicated in RA. Researchers identified them as prime targets for intervention. Setting the stage for the development of JAK inhibitors, including Baricitinib.
Baricitinib’s Mechanism of Action: Precision in Targeting JAK1 and JAK2:
Baricitinib’s journey is defined by its precision in targeting JAK1 and JAK2. As a JAK inhibitor, it disrupts the signalling cascade responsible for the dysregulated immune response characteristic of RA. By selectively inhibiting these key players in the inflammatory orchestra. Baricitinib provides a finely tuned intervention, offering the promise of modulating the immune system with a level of specificity previously unseen in RA therapeutics.
Regulatory Approval and Global Recognition:
The culmination of extensive preclinical and clinical research resulted in regulatory approvals that underscored the significance of Baricitinib in the RA landscape. The U.S. Food and Drug Administration (FDA), and the European Medicines Agency (EMA). Other regulatory bodies globally acknowledged the potential of Baricitinib. Granting it the status of a breakthrough therapy for those living with moderate to severe RA.
A Shifting Paradigm: Beyond Symptom Management to Disease Modification:
The introduction of Baricitinib represents a shift from conventional approaches focused on symptom management to a more ambitious goal—disease modification. The potential to alter the course of RA, inhibiting radiographic progression and improving physical function. Positions Baricitinib (Baricinix 2) as a beacon of hope for patients seeking transformative outcomes.
In conclusion, the background of Baricitinib is woven into the fabric of scientific exploration, and technological innovation. A commitment to addressing the unmet needs of individuals navigating the complexities of rheumatoid arthritis. As Baricitinib takes centre stage in the ongoing evolution of RA therapeutics, Its story reflects the collective pursuit of precision and efficacy in the quest to redefine the treatment paradigm for autoimmune diseases.
Mechanism of Action Baricitinib (Baricinix):
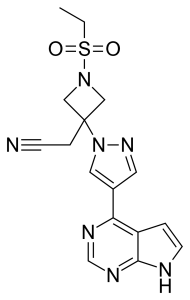
Baricitinib, a pioneering Janus kinase (JAK) inhibitor, orchestrates its transformative impact in the realm of rheumatoid arthritis (RA) by navigating the intricate molecular pathways that underlie inflammation and immune dysregulation. Understanding the nuances of Baricitinib’s mechanism of action reveals a story of precision, where the drug selectively disrupts key signalling events to curtail the relentless inflammatory cascade characteristic of RA.
1. Inhibiting Janus Kinases (JAKs) – A Strategic Intervention:
At the core of Baricitinib’s mechanism of action is its ability to inhibit specific Janus kinases—JAK1 and JAK2. These enzymes play a pivotal role in the JAK-STAT signaling pathway, a fundamental pathway in the regulation of immune responses. By selectively targeting JAK1 and JAK2, Baricitinib (Baricinix 2) acts as a molecular brake, disrupting the transmission of signals that drive the aberrant immune activity seen in RA.
2. Modulating Cytokine Signaling:
The JAK-STAT pathway is a critical mediator of cytokine signaling, including key players like interleukins (ILs) and interferons (IFNs). Baricitinib’s intervention in this pathway modulates the signaling of pro-inflammatory cytokines, such as IL-6 and interferon-gamma, which are implicated in the perpetuation of RA-associated inflammation. By dampening these signals, Baricitinib contributes to the attenuation of the destructive inflammatory processes within the joints.
3. Fine-Tuned Immune Response:
Baricitinib’s precision extends beyond mere inhibition, aiming for a fine-tuned modulation of the immune response. This nuanced approach allows the drug to selectively target pathological immune processes while preserving essential aspects of the body’s defense mechanisms. The goal is not only to alleviate symptoms but also to recalibrate the immune system’s behavior, addressing the root cause of RA.
4. Impact on Synovial Inflammation:
In RA, synovial inflammation is a hallmark feature, leading to joint destruction and functional impairment. Baricitinib’s intervention in the JAK-STAT pathway extends to the synovium, where it dampens the inflammatory milieu. This impact on the synovial microenvironment contributes to the drug’s ability to mitigate joint damage and improve the overall disease activity in RA patients.
5. Clinical Implications: Rapid Onset and Sustained Efficacy:
Baricitinib’s targeted mechanism of action is reflected in its clinical implications, including a rapid onset of action and sustained efficacy. Clinical trials have demonstrated its ability to provide swift relief from RA symptoms, making it a valuable therapeutic option for patients in need of prompt and effective intervention. Moreover, the sustained disease-modifying effects underscore its potential to alter the long-term course of RA.
As the symphony of inflammation in rheumatoid arthritis plays out, Baricitinib’s mechanism of action emerges as a harmonious composition of precision and efficacy. By selectively navigating the intricate pathways of the immune response, Baricitinib (Baricinix 2) stands as a testament to the potential of targeted therapies in reshaping the landscape of RA treatment, offering a melody of relief and hope to those affected by this complex autoimmune disorder.
Clinical Uses of Baricitinib (Baricinix):
Baricitinib, a Janus kinase (JAK) inhibitor, has emerged as a transformative agent in the clinical landscape of rheumatoid arthritis (RA), offering a multifaceted approach to disease management. Its clinical uses extend beyond mere symptom relief, encompassing disease modification and improving overall quality of life for individuals grappling with the complexities of RA.
**1. Moderate to Severe Rheumatoid Arthritis:
Baricitinib has found its primary niche in the treatment of moderate to severe RA. Approved for use in patients who have had an inadequate response to conventional disease-modifying antirheumatic drugs (DMARDs), Baricitinib (Baricinix 2) serves as a valuable addition to the therapeutic armamentarium. Whether used as monotherapy or in combination with methotrexate or other conventional DMARDs, it demonstrates robust efficacy in alleviating symptoms and improving joint function.
**2. Swift Relief from RA Symptoms:
One of the hallmark features of Baricitinib’s clinical utility is its rapid onset of action. Clinical trials have shown that patients often experience swift relief from pain, joint swelling, and morning stiffness. This characteristic makes Baricitinib an attractive option for those in need of prompt and effective intervention to manage the acute manifestations of RA.
**3. Disease Modification:
Beyond symptom control, Baricitinib has demonstrated disease-modifying effects, inhibiting radiographic progression in RA. This aspect is pivotal in altering the long-term course of the disease, preserving joint integrity, and mitigating the structural damage that often accompanies chronic RA.
**4. Combination Therapies:
Baricitinib’s versatility shines in its compatibility with various treatment modalities. It can be used in combination with conventional DMARDs, such as methotrexate, offering a synergistic approach to disease control. This flexibility allows healthcare providers to tailor treatment plans to the individual needs of RA patients, optimizing outcomes through strategic combinations.
**5. Adaptive Dosing:
The adaptability of Baricitinib is further highlighted by ongoing research exploring different dosing regimens. Investigations into intermittent dosing or dose adjustments aim to maximize efficacy while minimizing potential side effects. This nuanced approach reflects a commitment to refining and personalizing the use of Baricitinib (Baricinix 2) for each patient.
**6. Versatility in Patient Profiles:
Baricitinib’s clinical uses extend to a diverse spectrum of patients, including those who have not responded adequately to other biologic or targeted synthetic DMARDs. Its versatility in patient profiles positions it as a valuable option for individuals facing the challenges of RA, regardless of prior treatment history.
**7. Investigations Beyond RA:
The clinical exploration of Baricitinib is not confined to RA alone. Ongoing research investigates its potential applications in other autoimmune conditions, such as systemic lupus erythematosus and atopic dermatitis, signaling a potential expansion of its clinical uses across a broader range of inflammatory disorders.
In the dynamic landscape of rheumatoid arthritis management, Baricitinib (Baricinix 2) stands as a versatile and potent therapeutic tool. Its clinical uses span a spectrum from rapid symptom relief to disease modification, reflecting a comprehensive approach to addressing the multifaceted challenges posed by RA. As research continues to unfold, Baricitinib’s role in rheumatology promises to evolve, offering new possibilities for improved outcomes and enhanced quality of life for those navigating the complexities of autoimmune disease.
Clinical Trials and Research of Baricitinib (Baricinix):
Baricitinib, with its revolutionary role in rheumatoid arthritis (RA) treatment, owes much of its prominence to extensive clinical trials and ongoing research endeavors. These studies delve into the intricacies of Baricitinib’s efficacy, safety, and potential applications beyond RA, contributing to the evolving narrative of its place in the ever-expanding landscape of autoimmune disease therapeutics.
**1. Early Clinical Trials: Paving the Way:
The journey of Baricitinib (Baricinix 2) began with early-phase clinical trials that sought to establish its safety, tolerability, and preliminary efficacy. These foundational studies provided insights into optimal dosages, potential side effects, and the drug’s overall pharmacological profile. Building upon this groundwork, subsequent trials ventured into exploring its therapeutic potential in diverse patient populations.
**2. Phase III Trials: Efficacy Unveiled:
Phase III trials for Baricitinib (Baricinix 2) focused on large patient cohorts, aiming to definitively establish its efficacy in RA. These pivotal studies demonstrated Baricitinib’s ability to achieve significant reductions in disease activity, improve physical function, and inhibit radiographic progression when compared to conventional treatments. The pivotal RA-BEACON, RA-BEGIN, and RA-BUILD trials played instrumental roles in securing regulatory approvals for Baricitinib.
**3. Comparative Effectiveness Studies: Benchmarking Baricitinib:
Comparative effectiveness studies have sought to benchmark Baricitinib against other disease-modifying antirheumatic drugs (DMARDs) and biologics. These investigations provide valuable insights into the relative efficacy and safety of Baricitinib (Baricinix 2) in real-world scenarios, informing clinicians on its positioning within the broader landscape of RA therapeutics.
**4. Long-Term Extension Studies: Sustained Efficacy and Safety:
The durability of Baricitinib’s effects is a critical aspect under scrutiny in long-term extension studies. These trials aim to assess the sustained efficacy and safety of Baricitinib (Baricinix 2) over extended treatment durations. Providing crucial data on its ability to maintain disease control and manage potential side effects in the context of prolonged use.
**5. Pediatric and Adolescent Studies: Extending the Horizon:
Recognizing the potential applicability of Baricitinib beyond adult populations. Ongoing studies explore its safety and efficacy in pediatric and adolescent patients with juvenile idiopathic arthritis. These investigations seek to provide therapeutic options for younger individuals facing autoimmune challenges.
**6. Exploration in Systemic Lupus Erythematosus (SLE) and Atopic Dermatitis:
Baricitinib’s therapeutic potential extends beyond RA, with ongoing research exploring its efficacy in systemic lupus erythematosus (SLE) and atopic dermatitis. Clinical trials in these conditions aim to uncover new dimensions of Baricitinib’s immunomodulatory effects. Potentially expanding its clinical uses to a broader spectrum of autoimmune diseases.
**7. Investigations into Adaptive Dosing: Personalizing Treatment:
Recognizing the heterogeneity of patient responses, research into adaptive dosing regimens is underway. Studies exploring intermittent dosing or dose adjustments aim to personalize Baricitinib (Baricinix 2)treatment plans, optimizing efficacy while minimizing potential side effects.
As Baricitinib continues to make strides in reshaping RA therapy, ongoing clinical trials and research initiatives play a pivotal role in refining its clinical profile. From elucidating its long-term safety to exploring novel applications. These studies represent the collective effort of researchers, clinicians, and pharmaceutical innovators in unraveling the full therapeutic potential of Baricitinib in the intricate tapestry of autoimmune diseases.
Potential Side Effects of Baricitinib (Baricinix):
Baricitinib, while heralded for its transformative impact on rheumatoid arthritis (RA) treatment, is not without potential side effects. As with any medication, understanding these nuances is crucial for both patients and healthcare providers. Vigilant monitoring and informed management strategies are paramount in ensuring the balance between therapeutic benefits and potential risks associated with Baricitinib (Baricinix 2).
**1. Risk of Infections:
Baricitinib’s immunomodulatory effects may pose an increased risk of infections, including respiratory and urinary tract infections. Vigilance for signs of infection, coupled with proactive measures such as vaccinations, can help mitigate this potential side effect. Close communication between patients and healthcare providers is essential for early detection and intervention.
**2. Herpes Zoster Reactivation:
Herpes zoster (shingles) reactivation has been reported as a potential side effect of Baricitinib. Patients, especially those with a history of varicella zoster virus exposure, should be monitored for symptoms. Vaccination against herpes zoster prior to initiating Baricitinib is recommended in many cases to reduce the risk of reactivation.
**3. Gastrointestinal Perforations:
Rare but serious, gastrointestinal perforations have been noted in patients taking Baricitinib. Monitoring for signs such as abdominal pain, tenderness, and persistent vomiting is crucial. Prompt medical attention is imperative if these symptoms arise, as gastrointestinal perforations can lead to severe complications.
**4. Blood Cell Abnormalities:
Baricitinib (Baricinix 2) may impact blood cell counts, including a reduction in hemoglobin levels and lymphocyte counts. Regular blood monitoring is essential to detect and manage any abnormalities. Patients undergoing Baricitinib therapy should be aware of the importance of routine blood tests as part of their overall healthcare management.
**5. Elevated Liver Enzymes:
Baricitinib treatment has been associated with elevated liver enzymes. Regular monitoring of liver function is crucial to detect any signs of hepatotoxicity promptly. In cases where liver enzyme levels rise. Healthcare providers may adjust the treatment plan or recommend closer monitoring to ensure optimal liver health.
**6. Lipid Profile Changes:
Baricitinib has been linked to alterations in lipid profiles, including increases in cholesterol and triglyceride levels. Healthcare providers may monitor lipid levels and recommend lifestyle modifications or pharmacological interventions as necessary to manage these changes and mitigate cardiovascular risk.
**7. Hypertension:
Baricitinib (Baricinix 2) may contribute to increased blood pressure. Regular blood pressure monitoring and lifestyle modifications. Such as dietary changes and exercise, are integral components of managing this potential side effect. Antihypertensive medications may be considered based on individual patient needs.
**8. Risk of Thrombosis:
Thrombosis, including deep vein thrombosis and pulmonary embolism. Is a rare but serious potential side effect of Baricitinib. Patients with known risk factors for thrombosis should be closely monitored. Preventive measures may be implemented based on individual risk assessments.
As patients embark on Baricitinib therapy, collaborative and open dialogue with healthcare providers is essential. Proactive monitoring, early detection, and timely intervention contribute to a comprehensive and patient-centred approach. Ensuring that the potential side effects associated with Baricitinib are managed effectively. Allowing individuals to derive the maximum benefit from this innovative rheumatoid arthritis treatment.
Emerging Trends and Developments of Baricitinib (Baricinix):
As Baricitinib solidifies its standing as a transformative agent in rheumatoid arthritis (RA) treatment. Emerging trends and ongoing developments signify a dynamic evolution in its application and potential impact on patient care. Beyond its established role in RA. The horizon of Baricitinib’s therapeutic influence is expanding. Revealing novel opportunities and promising directions for its utilization.
**1. Extended Applications in Autoimmune Diseases:
The exploration of Baricitinib’s efficacy is not confined to RA alone. Ongoing research is expanding its applications to other autoimmune conditions, including systemic lupus erythematosus (SLE) and atopic dermatitis. These investigations aim to unravel the broader immunomodulatory potential of Baricitinib (Baricinix 2). Potentially paving the way for its adoption in a spectrum of autoimmune disorders.
**2. Combination Therapies and Synergies:
As researchers delve into optimizing treatment strategies, combination therapies involving Baricitinib are gaining prominence. Studies explore synergies between Baricitinib and other disease-modifying antirheumatic drugs (DMARDs) or biologics. Seeking enhanced efficacy and potentially more durable disease control. The goal is to tailor treatments for individual patients, addressing the complexities of diverse RA presentations.
**3. Pediatric Rheumatology: A Frontier in Exploration:
Baricitinib’s potential role in pediatric rheumatology is a burgeoning frontier in its developmental trajectory. Clinical trials are underway to evaluate its safety and efficacy in juvenile idiopathic arthritis. Offering hope for effective therapeutic options for children and adolescents grappling with autoimmune challenges.
**4. Precision Medicine and Biomarker Discovery:
The pursuit of precision medicine in RA treatment involves identifying biomarkers that can predict individual responses to Baricitinib. Ongoing research aims to unravel the genetic and molecular signatures associated with treatment outcomes. Paving the way for more personalized and targeted approaches. This approach holds promise in refining patient stratification and optimizing therapeutic benefits.
**5. Adaptive Dosing and Individualized Regimens:
The evolution of Baricitinib (Baricinix 2) research includes investigations into adaptive dosing regimens. Recognizing the heterogeneity in patient responses, researchers explore flexible dosing schedules or dose adjustments tailored to individual needs. These approaches seek to optimize therapeutic outcomes while minimizing potential side effects, aligning with the broader trend of personalized medicine.
**6. Real-World Evidence and Long-Term Safety:
Beyond controlled clinical trials. The accumulation of real-world evidence is shaping our understanding of Baricitinib’s long-term safety and effectiveness. Observational studies contribute valuable insights into its performance in diverse patient populations and under real-world conditions. Providing a more comprehensive view of its utility beyond the confines of clinical trials.
**7. Digital Health and Patient-Centric Approaches:
The integration of digital health tools and patient-centric approaches is emerging as a trend in Baricitinib’s utilization. Mobile applications, wearable devices, and telehealth interventions play roles in monitoring patient outcomes and enhancing adherence. Facilitating proactive communication between healthcare providers and individuals on Baricitinib therapy.
As Baricitinib evolves from a groundbreaking therapy to a multifaceted therapeutic entity. These emerging trends and developments underscore its dynamic trajectory in rheumatology and autoimmune disease management. From precision medicine to expanding applications and patient-centric approaches. The evolving landscape of Baricitinib research promises not only enhanced efficacy in existing indications but also a future where this innovative therapy plays a pivotal role in diverse autoimmune conditions and treatment modalities.
Conclusion of Baricitinib (Baricinix):
In the dynamic landscape of autoimmune disease therapeutics, Baricitinib (Baricinix 2) stands as a transformative force. Reshaping the narrative of rheumatoid arthritis (RA) treatment and venturing into new frontiers of clinical exploration. As we reflect on its journey and evolving role. Several key facets underscore Baricitinib’s enduring legacy and potential contributions to the broader field of autoimmune disorders.
**1. Revolutionizing RA Treatment:
Baricitinib’s approval and subsequent integration into clinical practice represent a paradigm shift in the approach to RA treatment. From its rapid onset of action to its disease-modifying effects. Baricitinib has become a cornerstone in the management of moderate to severe RA. Offering tangible benefits in terms of symptom relief, improved physical function, and inhibited radiographic progression.
**2. Expanding Applications Across Autoimmune Diseases:
The exploration of Baricitinib’s efficacy beyond RA marks an exciting chapter in its trajectory. Ongoing research in systemic lupus erythematosus (SLE), and atopic dermatitis. Juvenile idiopathic arthritis signifies the potential expansion of its therapeutic applications. Opening new possibilities for patients grappling with a spectrum of autoimmune challenges.
**3. Precision Medicine and Personalized Approaches:
The pursuit of precision medicine in the realm of RA therapy is exemplified by Baricitinib. Ongoing investigations into biomarker discovery and adaptive dosing regimens underscore a commitment to tailoring treatments to individual patient profiles. This precision-driven approach holds promise in optimizing therapeutic benefits and refining patient outcomes.
**4. Pediatric Rheumatology and Future Generations:
Baricitinib’s foray into pediatric rheumatology represents a significant stride in addressing autoimmune challenges in younger populations. As clinical trials unfold. The potential for Baricitinib (Baricinix 2) to become a therapeutic beacon for children and adolescents with autoimmune conditions adds a poignant chapter to its narrative.
**5. Real-World Impact and Long-Term Safety:
The accumulation of real-world evidence contributes valuable insights into Baricitinib’s long-term safety and effectiveness. Beyond the controlled environment of clinical trials. The real-world impact of baricitinib is shaping our understanding of its performance in diverse patient populations. Enriching the evidence base for its utilization.
**6. Digital Health Integration and Patient-Centric Care:
The integration of digital health tools and patient-centric approaches underscores a commitment to holistic and proactive care. Baricitinib’s journey includes the incorporation of mobile applications. Wearable devices, and telehealth interventions, foster a collaborative and informed partnership between patients and healthcare providers.
In conclusion, Baricitinib’s enduring legacy extends beyond its role as a groundbreaking therapy for RA. As it continues to evolve and diversify. Baricitinib embodies the spirit of innovation in autoimmune disease therapeutics. Its impact is not confined to a single condition but resonates across various autoimmune landscapes, offering hope, and relief. The prospect of a more personalized and targeted approach to patient care. As research progresses the story of Baricitinib unfolds. Its legacy in the ongoing quest for effective and transformative autoimmune disease treatments is poised to endure.