Gilteritinib (Gilternib)
Gilteritinib (Gilternib) Marketed under the brand name Gilternib, stands as a notable player in the landscape of targeted therapies. Particularly in the realm of hematologic malignancies. This innovative medication, classified as a tyrosine kinase inhibitor (TKI). Has become a critical tool in the treatment armamentarium, offering new avenues in the fight against specific forms of leukemia.
The primary indication for Gilteritinib (Gilternib) lies in the treatment of acute myeloid leukemia (AML) with a specific genetic mutation known as FLT3-ITD (internal tandem duplication) or FLT3-TKD (tyrosine kinase domain) mutations. These mutations are associated with a more aggressive course of AML and poorer outcomes. Gilteritinib’s mechanism of action involves selectively inhibiting the mutated FLT3 receptor. Disrupting the signaling pathways that contribute to the uncontrolled growth and survival of leukemia cells.
Clinical trials have demonstrated the efficacy of Gilteritinib (Gilternib) in improving response rates and prolonging survival in patients with FLT3-mutated AML.
Its approval represents a significant advancement in precision medicine, Tailoring treatment strategies to the specific genetic characteristics of individual tumors.
The convenience of oral administration adds to Gilteritinib’s appeal. Providing patients with a more accessible and patient-friendly mode of treatment. However, like many targeted therapies, Gilteritinib (Gilternib) is not without potential side effects. Close monitoring by healthcare professionals is crucial to managing any adverse reactions and optimizing treatment outcomes.
As research into the molecular underpinnings of cancer continues to evolve. Targeted therapies like Gilteritinib (Gilternib) remain at the forefront of the fight against hematologic malignancies. Their role in reshaping the treatment landscape reflects a commitment to providing effective. Personalized treatment options for individuals facing the challenges of specific genetic mutations in AML. In the ongoing quest for more effective and targeted cancer therapies, Gilteritinib (Gilternib) stands as a beacon. Illuminating the path toward innovative interventions for patients with FLT3-mutated AML.
Introduction of Gilteritinib (Gilternib):
Gilteritinib (Gilternib), a novel and promising therapeutic agent, has emerged as a beacon of hope in the realm of cancer treatment. Specifically for patients grappling with acute myeloid leukemia (AML). This tyrosine kinase inhibitor was developed and marketed under the brand name Xospata. Has demonstrated remarkable efficacy in targeting and inhibiting the activity of certain mutated proteins associated with AML. The approval of gilteritinib by regulatory authorities marks a significant stride in the ongoing quest for more effective. Targeted treatments for hematologic malignancies.
AML, characterized by the rapid growth of abnormal blood cells in the bone marrow, poses a formidable challenge in the oncology landscape. The conventional treatment approaches, such as chemotherapy and stem cell transplantation, have often proven to be arduous for patients and may not yield optimal outcomes. Gilteritinib (Gilternib), however, represents a paradigm shift by specifically addressing mutations in the FMS-like tyrosine kinase 3 (FLT3) gene, a common genetic alteration found in a substantial proportion of AML cases.
The FLT3 mutation, frequently observed in AML patients, leads to aberrant signaling pathways that contribute to the uncontrolled proliferation of leukemia cells.
Gilteritinib’s mechanism of action involves selectively inhibiting FLT3, thereby disrupting these signaling cascades and impeding the growth and survival of leukemia cells. This targeted approach holds the promise of enhancing treatment efficacy while minimizing the impact on normal, healthy cells, potentially mitigating the adverse effects associated with traditional chemotherapy.
Clinical trials evaluating the safety and efficacy of Gilteritinib (Gilternib) have yielded encouraging results, leading to its approval for the treatment of relapsed or refractory FLT3-positive AML. Furthermore, ongoing research is exploring its potential in combination with other therapies and its applicability in the frontline setting.
This article delves into the intricacies of gilteritinib, exploring its pharmacology, clinical applications, and the evolving landscape of FLT3-targeted therapies. As we navigate the nuances of this groundbreaking agent, it becomes apparent that Gilteritinib (Gilternib) represents a beacon of optimism for AML patients and a testament to the advancements in precision medicine within the oncology field.
Background of Gilteritinib (Gilternib):
Gilteritinib (Gilternib), a potent and highly selective inhibitor of FMS-like tyrosine kinase 3 (FLT3), has emerged as a pivotal player in the landscape of targeted therapies for acute myeloid leukemia (AML). The genesis of gilteritinib can be traced to the imperative need for more effective and tailored treatments, particularly in the context of AML cases harboring FLT3 mutations.
FLT3, a receptor tyrosine kinase, plays a crucial role in regulating the growth and survival of hematopoietic cells. Mutations in the FLT3 gene, commonly observed in AML, result in constitutive activation of the receptor, leading to uncontrolled cell proliferation and a more aggressive disease course. Recognizing the significance of FLT3 mutations in AML pathogenesis, researchers sought to develop targeted therapies to disrupt the aberrant signaling pathways associated with these mutations.
Gilteritinib (Gilternib), with its potent inhibitory activity against both FLT3-ITD (internal tandem duplication) and FLT3-TKD (tyrosine kinase domain) mutations, represents a breakthrough in this endeavor. The drug’s ability to selectively target and inhibit mutated FLT3 receptors distinguishes it from conventional chemotherapy, offering a more precise and less toxic approach to AML treatment.
The development of Gilteritinib (Gilternib) was propelled by a series of preclinical studies demonstrating its efficacy in suppressing leukemia cell proliferation and inducing apoptosis.
These promising findings laid the groundwork for clinical trials aimed at evaluating the safety and efficacy of gilteritinib in AML patients, particularly those with relapsed or refractory disease.
Notably, the pivotal ADMIRAL trial played a pivotal role in establishing the efficacy of gilteritinib. The trial demonstrated a significant improvement in overall survival for patients receiving gilteritinib compared to standard salvage chemotherapy, solidifying its place as a groundbreaking therapeutic option for FLT3-positive AML.
The approval of Gilteritinib (Gilternib) by regulatory agencies marked a pivotal moment in the journey of precision medicine in AML. As gilteritinib continues to evolve from a promising experimental agent to a standard of care, ongoing research endeavors are exploring its potential in various treatment settings, including combination therapies and its use in newly diagnosed patients.
In the backdrop of its targeted mechanism of action and promising clinical outcomes, Gilteritinib (Gilternib) stands as a beacon of hope for AML patients, offering not only improved survival but also a glimpse into the future of precision oncology. The following sections will delve into the pharmacological nuances, clinical applications, and future directions of gilteritinib in the context of AML management.
Mechanism of Action Gilteritinib (Gilternib):
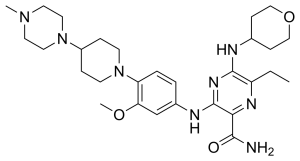
Gilteritinib (Gilternib), a potent and highly selective tyrosine kinase inhibitor, exerts its therapeutic effects through meticulously orchestrated interference with the aberrant signaling pathways associated with FLT3 mutations in acute myeloid leukemia (AML). The mechanism of action of gilteritinib lies in its ability to specifically target and inhibit both FLT3-ITD (internal tandem duplication) and FLT3-TKD (tyrosine kinase domain) mutations, pivotal drivers of leukemic cell proliferation and survival.
The FMS-like tyrosine kinase 3 (FLT3) receptor, a transmembrane protein expressed on the surface of hematopoietic progenitor cells, plays a critical role in regulating normal cell growth and differentiation. In the context of AML, mutations in the FLT3 gene lead to constitutive activation of the receptor, triggering downstream signaling cascades that contribute to the uncontrolled proliferation of leukemia cells.
Gilteritinib (Gilternib) disrupts this pathological signaling by binding to the adenosine triphosphate (ATP)-binding pocket of FLT3, thereby inhibiting its kinase activity.
This targeted inhibition impedes the phosphorylation of downstream signaling molecules, including STAT5, MAPK, and AKT, which are crucial for the survival and proliferation of leukemia cells. By stifling these signaling pathways, gilteritinib exerts a profound antileukemic effect, inducing apoptosis and halting the unbridled expansion of malignant cells.
Furthermore, the dual inhibition of both FLT3-ITD and FLT3-TKD mutations distinguishes gilteritinib from earlier FLT3 inhibitors, broadening its applicability to a wider spectrum of FLT3-altered AML cases. This selectivity is crucial in mitigating off-target effects and optimizing the drug’s efficacy in patients with diverse FLT3 mutations.
Clinical trials, particularly the landmark ADMIRAL trial, underscored the clinical significance of gilteritinib’s mechanism of action. Patients with relapsed or refractory FLT3-positive AML receiving gilteritinib demonstrated not only superior response rates but also a marked improvement in overall survival compared to those treated with standard salvage chemotherapy.
The precision and selectivity of gilteritinib’s mechanism of action align with the evolving paradigm of personalized cancer therapy, highlighting the potential for targeted treatments to improve outcomes while minimizing the adverse effects associated with traditional chemotherapy. As research endeavors continue to unravel the intricacies of FLT3 signaling and its role in AML, gilteritinib stands as a beacon of progress, offering a targeted and effective therapeutic option for patients grappling with this challenging hematologic malignancy.
Clinical Uses of Gilteritinib (Gilternib):
Gilteritinib (Gilternib), a potent FLT3 tyrosine kinase inhibitor, has established itself as a key player in the therapeutic arsenal against acute myeloid leukemia (AML), particularly in cases characterized by FLT3 mutations. The clinical utility of gilteritinib extends across several contexts, showcasing its efficacy and potential to redefine treatment paradigms in AML.
Relapsed or Refractory FLT3-Positive AML:
The primary and FDA-approved indication for gilteritinib is in the treatment of relapsed or refractory AML with FLT3 mutations. AML patients harboring FLT3 alterations often face a more aggressive disease course and a higher likelihood of relapse. Gilteritinib’s targeted inhibition of mutated FLT3 receptors disrupts the aberrant signaling pathways, impeding leukemic cell growth and offering a beacon of hope for patients who have experienced treatment failure with conventional therapies.
Post-Transplant Maintenance:
Gilteritinib’s role extends beyond the initial treatment phase. In the post-hematopoietic stem cell transplantation (HSCT) setting, where patients are vulnerable to disease relapse. Gilteritinib is being investigated as a potential maintenance therapy. By inhibiting residual leukemia cells post-transplant, gilteritinib aims to mitigate the risk of disease recurrence. Providing a proactive strategy to enhance long-term remission rates.
Combination Therapies:
The dynamic landscape of AML treatment is witnessing the integration of Gilteritinib (Gilternib) into combination therapies. Clinical trials exploring synergistic effects with conventional chemotherapy, hypomethylating agents, or other targeted therapies are underway. These combinations seek to capitalize on the strengths of different treatment modalities, potentially improving response rates and addressing the heterogeneity of AML.
Frontline Treatment (Investigational):
Gilteritinib’s success in relapsed or refractory settings has sparked interest in its potential as a frontline treatment. Ongoing investigations are exploring the feasibility of incorporating gilteritinib into initial treatment regimens for AML. If proven effective, this could reshape the landscape of first-line therapies, providing a targeted and well-tolerated option from the outset of AML diagnosis.
Pediatric AML:
Gilteritinib’s application extends to pediatric AML, where FLT3 mutations also play a role in disease pathogenesis. Clinical trials are assessing the safety and efficacy of gilteritinib in children, with the aim of addressing the unique challenges and requirements of pediatric leukemia treatment.
As gilteritinib continues to undergo exploration in diverse clinical scenarios, its versatility and targeted approach underscore its potential to redefine standards of care and improve outcomes for a broad spectrum of AML patients.
Clinical Trials and Research of Gilteritinib (Gilternib):
The journey of Gilteritinib (Gilternib) from experimental compound to FDA-approved therapy has been shaped by a robust portfolio of clinical trials and ongoing research endeavors. These studies, meticulously designed to evaluate gilteritinib’s safety, efficacy. Potential applications have played a pivotal role in shaping its current status as a groundbreaking treatment for acute myeloid leukemia (AML).
ADMIRAL Trial:
The pivotal ADMIRAL trial stands as a landmark study that paved the way for gilteritinib’s regulatory approval. Focused on relapsed or refractory FLT3-positive AML, the trial compared gilteritinib with standard salvage chemotherapy. Results demonstrated a clear advantage for gilteritinib, showcasing not only improved response rates but, critically, a significant extension in overall survival. This trial solidified gilteritinib as a transformative option for patients facing the challenges of treatment-resistant AML.
QuANTUM-First Trial:
The QuANTUM-First trial delves into the investigational use of gilteritinib as a frontline treatment for newly diagnosed AML patients with FLT3 mutations. This study explores the potential of gilteritinib to redefine first-line therapeutic strategies. Aiming to establish its efficacy and safety profile in a broader patient population.
ACE-536 and Gilteritinib Combination Studies:
Combinatorial approaches are at the forefront of AML research, and ongoing studies are investigating the synergies between gilteritinib and other therapeutic agents. Notably, combination studies with ACE-536, a molecule targeting the transforming growth factor-beta (TGF-β) pathway. Seek to enhance the efficacy of gilteritinib by addressing potential resistance mechanisms and optimizing treatment outcomes.
Pediatric Clinical Trials:
Recognizing the unique challenges posed by pediatric AML. Clinical trials are underway to assess the safety and efficacy of gilteritinib in children. These studies aim to extend the benefits of gilteritinib to the pediatric population. Addressing the critical need for targeted therapies in young patients with FLT3-mutated leukemia.
Post-Transplant Maintenance Studies:
Investigational studies exploring gilteritinib as a post-transplant maintenance therapy are focused on preventing disease relapse in AML patients who have undergone hematopoietic stem cell transplantation. These trials aim to redefine post-transplant care strategies, potentially improving long-term outcomes for patients vulnerable to disease recurrence.
These ongoing clinical trials and research initiatives underscore the commitment to unraveling the full potential of gilteritinib across various treatment scenarios. As the scientific community continues to delve into the nuances of AML biology and treatment responses. The results of these studies hold the promise of further refining and expanding the clinical applications of gilteritinib in the evolving landscape of leukemia therapeutics.
Potential Side Effects of Gilteritinib (Gilternib):
While Gilteritinib (Gilternib) has demonstrated remarkable efficacy in the treatment of acute myeloid leukemia (AML). Like any therapeutic agent, it comes with potential side effects. Understanding these side effects is crucial for healthcare professionals and patients alike to ensure vigilant monitoring and prompt management. It’s important to note that not all individuals will experience these side effects, and their severity can vary. Patients undergoing gilteritinib treatment should have open communication with their healthcare team to address any concerns promptly.
Cardiac Effects:
Gilteritinib (Gilternib) has been associated with QT interval prolongation, a cardiac electrophysiological alteration that could increase the risk of arrhythmias. Patients with a history of QT prolongation, and those taking medications that may affect QT interval. Those with pre-existing heart conditions may require close cardiac monitoring during gilteritinib therapy.
Myelosuppression:
Myelosuppression, a hallmark of gilteritinib treatment, is characterized by a decrease in blood cell counts, including thrombocytopenia, neutropenia, and anemia. To safeguard against this adverse effect, regular blood tests are essential to meticulously monitor blood cell levels. Consequently, appropriate interventions, such as dose adjustments or supportive care, can be swiftly implemented if myelosuppression emerges.
Liver Function Abnormalities:
Elevated liver enzymes have been reported in some patients receiving gilteritinib. Regular liver function tests are recommended to monitor for potential hepatotoxicity. If liver enzyme levels become elevated, dose adjustments or temporary discontinuation may be necessary.
Pancreatitis:
Gilteritinib has been associated with pancreatitis, which may present with symptoms such as abdominal pain, and nausea. Vomiting. Close monitoring for signs of pancreatitis is crucial, and appropriate interventions. Including treatment discontinuation, may be considered if pancreatitis is suspected.
Posterior Reversible Encephalopathy Syndrome (PRES):
While rare, cases of Posterior Reversible Encephalopathy Syndrome (PRES) have been reported with gilteritinib. Symptoms may include headaches, seizures, visual disturbances, and altered mental function. Prompt recognition and management are essential in suspected cases of PRES.
Interstitial Lung Disease (ILD):
ILD, characterized by inflammation and scarring of the lung tissue, is a potential side effect of gilteritinib. Patients experiencing symptoms such as cough, dyspnea, or fever should undergo evaluation. Treatment may need to be adjusted or discontinued based on the severity of ILD.
Gastrointestinal Effects:
Gilteritinib may cause gastrointestinal side effects, including nausea, diarrhea, and vomiting. Supportive measures. Such as antiemetics and dietary modifications, may be employed to manage these symptoms.
Healthcare providers need to educate patients undergoing gilteritinib treatment about these potential side effects. Stay vigilant in monitoring and managing these issues. Individualized assessment and a collaborative approach between patients and healthcare teams are crucial to optimizing the benefits of gilteritinib while minimizing the impact of potential side effects.
Emerging Trends and Developments of Gilteritinib (Gilternib):
The landscape of Gilteritinib (Gilternib) and its applications in the realm of acute myeloid leukemia (AML) is dynamic. Marked by ongoing research and evolving clinical paradigms. Several emerging trends and developments are shaping the future trajectory of gilteritinib and its role in the management of AML.
Frontline Combination Therapies:
A notable trend in gilteritinib research involves exploring its potential as a frontline therapy in combination with other agents. Clinical trials are investigating the efficacy of gilteritinib in conjunction with standard induction therapies for newly diagnosed AML patients. The goal is to optimize treatment responses, and improve outcomes. Potentially deepen the pool of patients who can benefit from this targeted therapy from the outset of diagnosis.
Pediatric Applications:
As research expands, there is a growing focus on extending the use of gilteritinib to pediatric populations. Clinical trials dedicated to studying the safety and efficacy of gilteritinib in children with FLT3-mutated AML aim to address the unique challenges and treatment considerations in the pediatric oncology landscape.
MRD (Minimal Residual Disease) Assessment:
The assessment of Minimal Residual Disease (MRD) is becoming a critical component in the evaluation of treatment responses in AML. Emerging studies are investigating the role of gilteritinib in achieving and maintaining MRD negativity. Aiming to refine treatment strategies and potentially tailor therapeutic approaches based on residual disease burden.
Exploration of Combinatorial Approaches:
Beyond the established combination studies, ongoing research is exploring novel combinatorial approaches involving gilteritinib. Combinations with immune checkpoint inhibitors, epigenetic modifiers, and other targeted agents are under investigation. With the goal of addressing the heterogeneity of AML and overcoming resistance mechanisms.
Real-world Evidence and Long-Term Outcomes:
As gilteritinib gains wider acceptance in everyday medical settings. There is a mounting need to gather real-world data to supplement the findings of controlled clinical trials. Long-term follow-up studies are essential to assess the durability of responses. Understand potential late toxicities, and inform treatment decisions in diverse patient populations.
Biomarker Exploration:
Advancements in molecular profiling and biomarker discovery are shaping the era of precision medicine. Researchers are exploring additional biomarkers beyond FLT3 mutations that may influence responses to gilteritinib. These efforts aim to refine patient selection criteria. Personalize treatment approaches, and enhance the overall effectiveness of gilteritinib in AML.
Patient-reported Outcomes:
Recognizing the importance of patient experience, emerging trends include a focus on patient-reported outcomes. Studies are incorporating patient perspectives to understand the impact of gilteritinib on quality of life, and treatment tolerability. Long-term survivorship, providing a holistic view of its role in the patient journey.
As gilteritinib continues to evolve, these emerging trends and developments underscore the commitment of the scientific community to maximize the therapeutic potential of this agent. The convergence of innovative research, and personalized medicine principles. A patient-centered approach is poised to shape the future landscape of AML treatment with gilteritinib.
Conclusion of Gilteritinib (Gilternib):
In conclusion, gilteritinib has emerged as a transformative force in the realm of acute myeloid leukemia (AML), illuminating a path of hope for patients confronting the hurdles of FLT3-mutated disease. Its journey from experimental compound to FDA-approved therapy has been marked by a series of pivotal clinical trials. Demonstrating its efficacy and reshaping the paradigm of precision medicine in AML treatment.
The clinical uses of gilteritinib. Range from its established role in relapsed or refractory FLT3-positive AML to investigational applications in frontline therapy and post-transplant maintenance. Underscore its versatility and potential to redefine standards of care. The ongoing exploration of combination therapies, and pediatric applications. Its impact on minimal residual disease assessment reflects the dynamic nature of gilteritinib research. Emphasizing a commitment to refining treatment strategies and improving outcomes.
As gilteritinib becomes an integral part of AML management, the nuanced understanding of its mechanism of action. Potential side effects and the exploration of emerging trends collectively contribute to a comprehensive. View of its role in the evolving landscape of leukemia therapeutics. The patient-centric approach is evidenced by ongoing research into real-world outcomes and patient-reported experiences. Ensures a holistic understanding of gilteritinib’s impact on the lives of individuals navigating the complexities of AML.
Looking forward, gilteritinib stands poised at the forefront of advancements in AML treatment. Where personalized medicine principles and innovative research converge to shape the future of leukemia therapeutics. The strides made in understanding gilteritinib’s applications. It’s synergies with other agents. Its potential impact on long-term survivorship positions it as a cornerstone in the ongoing pursuit of more effective and tailored treatments for AML. As the journey continues, gilteritinib embodies the spirit of progress. Gilteritinib’s potential extends beyond mere survival; it offers a glimpse into a future where precision oncology transforms the landscape for patients battling hematologic malignancies.