In the realm of hepatology, Obeticholic Acid (OCA) emerges as a therapeutic protagonist, weaving a narrative of promise and innovation in the management of liver disorders. This active article embarks on a comprehensive exploration of Obeticholic Acid, unravelling its origins, mechanism of action, clinical applications, ongoing research endeavours, potential side effects, and its role in shaping the evolving landscape of hepatology.
Introduction of Obeticholic Acid (FXR):
In the intricate tapestry of hepatology, one compound has risen to prominence as a beacon of therapeutic innovation: Obeticholic Acid (FXR) (OCA).
Originally conceived as a targeted intervention for primary biliary cholangitis (PBC), Obeticholic Acid (FXR) has evolved beyond its initial scope, weaving a narrative of promise and exploration in the broader landscape of liver disorders. This introduction sets the stage for a comprehensive exploration of Obeticholic Acid, delving into its origins, mechanism of action, clinical applications, ongoing research endeavours, potential side effects, and its pivotal role in shaping the future of hepatology.
Origins and Evolution:
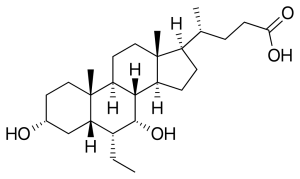
Obeticholic Acid’s journey begins with its roots in the synthetic modification of chenodeoxycholic acid, a naturally occurring bile acid. Developed with the primary goal of addressing the unique challenges posed by PBC, Obeticholic Acid’s evolution is marked by a trajectory that transcends its original purpose. As scientific understanding and clinical needs converge, Obeticholic Acid emerges as a multifaceted therapeutic agent with the potential to impact a spectrum of liver disorders.
Mechanism of Action:
At the molecular level, Obeticholic Acid engages in a complex dance with the farnesoid X receptor (FXR), orchestrating downstream effects that influence hepatic metabolism and bile acid synthesis. This sophisticated mechanism positions Obeticholic Acid as a targeted intervention, modulating lipid metabolism, inflammation, and fibrosis—a molecular symphony that holds promise in the intricate landscape of liver disorders.
Clinical Applications Beyond PBC:
While Obeticholic Acid found its initial application in PBC, ongoing clinical investigations are expanding its horizons. The potential applications of Obeticholic Acid now extend to nonalcoholic steatohepatitis (NASH), primary sclerosing cholangitis (PSC), and other liver disorders. The clinical tapestry of Obeticholic Acid unfolds as it emerges as a therapeutic ally in diverse hepatologic scenarios.
Navigating Clinical Trials and Research:
Obeticholic Acid’s narrative is interwoven with the threads of clinical trials and ongoing research endeavours. From pivotal trials establishing its efficacy in PBC to investigations exploring its impact on NASH, the evidence base supporting Obeticholic Acid’s role in liver therapeutics is dynamic and evolving. Ongoing research initiatives are pushing the boundaries of our understanding, revealing new facets of Obeticholic Acid’s potential impact.
Balancing Therapeutic Gains and Potential Side Effects:
As with any therapeutic agent, Obeticholic Acid is not without potential side effects. From pruritus and gastrointestinal symptoms to considerations about lipid metabolism, understanding and managing these adverse events are integral components of its clinical application. This delicate balance between therapeutic gains and patient tolerability is a key aspect of Obeticholic Acid’s role in liver disorders.
Emerging Trends and Developments:
In the ever-evolving landscape of hepatology, Obeticholic Acid stands at the nexus of emerging trends and developments. Its role in combination therapies, potential applications in pediatric liver disorders, and ongoing explorations point toward a future where Obeticholic Acid continues to shape the landscape of liver therapeutics.
In conclusion, Obeticholic Acid emerges as a trailblazer in hepatology—a compound with roots in targeted interventions for PBC that has evolved into a multifaceted therapeutic agent. Its journey reflects a commitment to addressing unmet clinical needs and pushing the boundaries of therapeutic possibilities. As Obeticholic Acid continues to weave its narrative, it beckons a future where liver disorders are met with targeted and effective interventions, offering hope to patients and reshaping the landscape of hepatology.
Background of Obeticholic Acid (FXR):
Obeticholic Acid (OCA) emerges from a rich tapestry of scientific inquiry, born out of a nuanced understanding of bile acids and their role in liver physiology. Its journey from conceptualization to clinical application is rooted in the persistent exploration of therapeutic avenues for liver disorders, with a primary focus on addressing the unique challenges posed by primary biliary cholangitis (PBC).
Bile Acids and Hepatic Physiology:
The story of Obeticholic Acid begins with bile acids, essential molecules with multifaceted roles in hepatic physiology. Bile acids are not merely digestive agents; they are intricately involved in the regulation of lipid metabolism, inflammation, and fibrosis within the liver. The exploration of bile acids as potential therapeutic targets reflects a deep appreciation for the interconnected pathways that govern liver function.
Chenodeoxycholic Acid and Synthetic Derivatives:
Obeticholic Acid is a synthetic derivative of chenodeoxycholic acid, a naturally occurring bile acid. Chenodeoxycholic acid itself has a storied history in hepatology, and its modification laid the groundwork for the development of Obeticholic Acid. This synthetic derivative was meticulously crafted to harness the beneficial aspects of chenodeoxycholic acid while optimizing its pharmacological properties for therapeutic efficacy.
Targeting Primary Biliary Cholangitis (PBC):
The genesis of Obeticholic Acid is intimately tied to the quest for effective interventions in primary biliary cholangitis. PBC, a chronic autoimmune liver disease characterized by the destruction of bile ducts, presented a formidable challenge in need of targeted solutions. Obeticholic Acid emerged as a potential answer, designed to modulate bile acid synthesis, promote hepatoprotective effects, and address the underlying pathophysiology of PBC.
Evolution Beyond PBC:
While PBC was the initial focal point, Obeticholic Acid’s journey has transcended its original boundaries. Ongoing research has broadened its horizons, exploring its potential applications in a spectrum of liver disorders. The evolution of Obeticholic Acid reflects a commitment to adapt and address the diverse clinical needs present in the complex landscape of hepatology.
Regulatory Milestones and Clinical Recognition:
Obeticholic Acid’s progression from experimental compound to a recognized therapeutic agent is marked by regulatory milestones and clinical recognition. Approvals from regulatory agencies underscore its safety and efficacy, providing clinicians with a valuable tool in the arsenal against liver disorders. Clinical recognition further solidifies Obeticholic Acid’s role as a pivotal intervention in the management of specific liver conditions.
In conclusion, the background of Obeticholic Acid is intricately woven with threads of scientific curiosity, synthetic innovation, and a commitment to addressing the complexities of liver disorders. From its roots as a derivative of chenodeoxycholic acid to its evolution beyond PBC, Obeticholic Acid stands as a testament to the pursuit of precision in hepatology—a pursuit that continues to shape its role in the evolving landscape of liver therapeutics.